If you’re in the process of treating severe ulcerative colitis (UC), surgery might sound like a scary step. But options like J-pouch surgery can help treat your UC symptoms without requiring major lifestyle changes.
After someone with UC gets their large intestine surgically removed, they might also undergo ileoanal anastomosis (aka J-pouch surgery) to help them eliminate waste via the usual route without a stoma or ostomy pouch.
What’s J-pouch surgery?
J-pouch surgery involves removing both the rectum and the colon. The surgeon then creates a J-shaped pouch from the end of the small intestine to help move waste through the body and out of the anus.
This surgery helps people avoid the need for a surgical opening in the abdomen for a stoma or ostomy pouch to manually eliminate waste.
Someone might get J-pouch surgery for any of these reasons:
- Treating chronic ulcerative colitis (UC). Most often, this procedure is used to treat chronic UC-related conditions, which carry a pretty big risk of colon or rectal cancer. J-pouch surgery is the most common procedure used to treat UC.
- Failure of UC meds. It’s typically recommended only when UC medications fail to control the condition. Then, J-pouch surgery may be the next method of treatment.
- Treating cancerous or precancerous conditions. J-pouch surgery is sometimes performed to treat colon or rectal cancer or as a preventive measure when precancerous changes are detected.
- Addressing emergency conditions. J-pouch surgery is sometimes performed in emergency situations such as uncontrolled gastrointestinal bleeding (a rare condition that can be life threatening) or toxic megacolon (which can lead to colon rupture if untreated).
You might be a candidate for J-pouch surgery if:
- your UC symptoms have persisted despite medication
- your UC symptoms are getting worse
- UC causes you to miss multiple days of school, work, or daily activities
- you have precancerous colon cells
- you have colon or rectal cancer
- you’re experiencing uncontrollable bleeding from your colon
- your doctor has found holes in your colon due to chronic inflammation
- you need surgery to remove your colon, but you’d rather have an internal pouch to collect waste than an external one
- you and your doctor decide that the procedure’s benefits outweigh the potential risks
What are the pros and cons of J-pouch surgery compared to ostomy procedures?
Folks often opt for J-pouch surgery over other procedures to treat UC because the J-pouch means you don’t need an external bag to collect waste.
After full recovery from J-pouch surgery, you won’t need to wear a stoma or empty it, and you’ll have more natural control over your bowel movements.
Pre-surgery prep
Before your surgery, your doctor will outline the risks of the procedure and what to expect. You’ll undergo a complete physical exam, which may include any of the following tests to ensure it’s the right option for you:
- blood work
- EKG
- colonoscopy
- chest X-ray
- rectal manometry
- upper GI X-rays
Your doctor will also address any concerns you have and give you the lowdown on what to expect, including a lesson on how to use your temporary stoma bag. You also may talk with an anesthesiologist about your pain management preferences.
In most cases, the procedure will take 6 to 10 hours and you’ll need to stay in the hospital for 5 to 10 days.
During surgery: The three stages
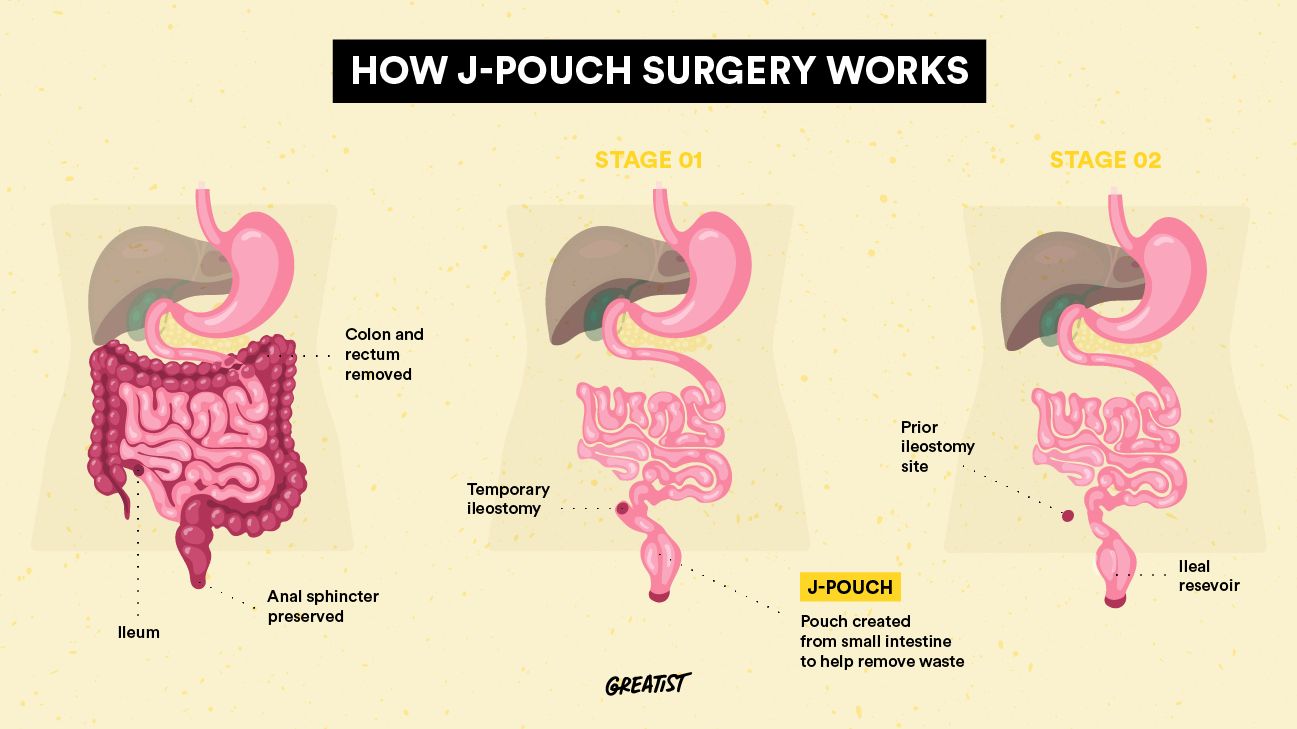
J-pouch surgery is typically completed in at least two stages. This allows time for healing and reduces the risk of infection compared to a single-stage procedure.
The first stage of J-pouch surgery looks like this:
- The surgeon removes your rectum and colon.
- The surgeon converts a portion of your small intestine (called the ileum) into a J-shaped “pouch.”
- To allow time for the J-pouch to heal, the surgeon usually makes a temporary ileostomy, or opening in your abdominal wall. A loop of your small intestine will pull through the opening to create a stoma, where waste can be removed from your body in the interim.
Once the J-pouch has healed (typically in 2 to 3 months), the second stage goes like this:
- The surgeon removes the temporary ileostomy/stoma bag.
- The surgeon reconnects the ileum of your small intestine to the J-pouch. The waste will now collect in the J-pouch. Stools can then pass normally through the anus.
In some cases, a third stage involves connecting the J-pouch directly to the anus for easier waste removal. This stage of surgery is needed if:
- you’re experiencing excessive bleeding
- you’re experiencing toxic megacolon
- you’re taking high doses of steroids
- you’re in poor health
Recovery and aftercare
After J-pouch surgery, you might experience a temporary increase in bowel movements — as many as 12 times a day. After several months, moving and grooving should return to normal as your anal sphincter muscles get stronger.
Your doc might recommend that you wait at least 6 weeks before resuming physical activity, depending on how well your GI tract heals after surgery.
After J-pouch surgery, people tend to have fewer UC symptoms, including:
- stool issues
- stomach pain or discomfort
- bloody stools
- fatigue
Like most other major operations, J-pouch surgery comes with potential risks. These include:
- Infections. Though infections are less common with multistep operations, they can still happen.
- Excess bleeding. If excessive bleeding happens after surgery, an emergency procedure may be necessary.
- Small bowel obstruction. This less common complication can happen when fibrous bands grow between tissues after surgery, causing nausea, vomiting, or an inability to go to the bathroom. In about two-thirds of cases, it can be treated with bowel rest (not eating for a few days and taking IV fluids). Other cases may require surgery.
- Pouchitis. This is inflammation of the J-pouch, which happens to an estimated 50 percent of people who have this surgery. Symptoms like fever, diarrhea, and abdominal pain are typically successfully treated with antibiotics.
- Pouch failure. In some cases, your body may reject the J-pouch and your doctor may instead recommend a stoma. The J-pouch would then need to be surgically removed.
- Phantom rectum. Phantom rectum may cause pain or the feeling of needing to pass stools even though you no longer have a rectum. Pain medication, guided imagery therapy, and antidepressants may help treat this.
- Sexual dysfunction. Nerve damage may sometimes lead to sexual issues (such as an absence of sensation).
- Infertility. Infertility may sometimes occur in females due to the scar tissue that grows around fallopian tubes and ovaries.
Research that followed 409 people through J-pouch surgery from 1981 to 1996 found that the procedure was successful for 91 percent of folks. In a small study of 39 people between 1987 and 2015, 3.5 to 15 percent experienced J-pouch failure.
Overall, the outlook seems good for a successful J-pouch surgery, but the available studies are either dated or small, so the actual success rate of the procedure is a bit of a mystery. Talk with your doctor about the specific risk factors that may apply to you.
If you do experience a pouch failure, the J-pouch will need to be surgically removed and a stoma will need to be used instead.
The most common side effect of J-pouch surgery is pouchitis (or J-pouch inflammation), which is treatable with antibiotics and typically doesn’t lead to pouch failure.
If you’re not a candidate for J-pouch surgery, if you need a wait a long time for surgery, or if you just want to ease your UC symptoms, you may want to try nonsurgical remedies such as:
- Dietary changes. Since certain foods can worsen UC symptoms, diet changes can help. Avoiding common trigger foods like dairy, caffeine, alcohol, juices, fried foods, spicy foods, red meat, and artificial colors and sweeteners might help. Your doc might also recommend a UC diet such as a low FODMAP diet.
- Medication. Your doctor might prescribe amino salicylates, corticosteroids, immunomodulators, or biologics to stop or ease symptoms. They might also prescribe pain relievers, antibiotics, or medication that minimizes colon spasms.
- Probiotics. UC involves an imbalance of “good” and “bad” bacteria in your large intestine, and there’s some evidence that probiotics might help remedy this. While we need more research to know for sure, at the very least, they probably can’t hurt.
J-pouch surgery is the most common treatment for UC. It involves removing the rectum and colon and creating a J-shaped pouch with the small intestine to allow waste to move through the anus as usual.
If your UC doesn’t respond to medication or other treatments and you don’t want an external ostomy, J-pouch surgery may be right for you.
As with any major surgery, you’ll want to discuss the potential benefits and risks with your doctor.
