Any kind of dry, irritated skin can be annoying AF. But facial psoriasis is next-level sucky and can feel like your face is under attack.
What is facial psoriasis anyways?
Psoriasis is a chronic skin condition that makes your skin cells multiply faster than normal. The excess skin cells pile up and create red scaly patches.
It affects more than 8 million Americans a year, and flare-ups can pop up anywhere on the bod. (Sorry friends, this includes your face.) In fact, about 50 percent of peeps with psoriasis will experience facial psoriasis.
Wondering if your irritated skin is actually facial psoriasis? Here’s how to decipher the symptoms, and top-notch treatments that can help keep your facial psoriasis in check.
Facial psoriasis is usually reddish or purplish in color, depending on your skin tone. You may also have silver or white scaling on the edges of the lesions. If it affects your peepers, you may experience visible inflammation or crusting 👀.
Facial psoriasis is most common on the:
- ears
- neck
- eyelids
- hairline
- forehead
- skin between nose and upper lip
- eyebrows
Due to its appearance, facial psoriasis sometimes gets mixed up with other skin conditions like dandruff, dry skin, eczema, or even herpes. But it’s def its own thing.
Flare-ups can also be super hard to predict. Some can last for weeks or even months before they chill out.
True facial psoriasis
True facial psoriasis plaques can show up anywhere on your face and tend to be symmetrical. It’s often associated with psoriasis on other parts of the body like the ears, genitals, elbows, knees, or scalp.
Sebopsoriasis
This is where seborrheic dermatitis and psoriasis meet. The result? Patchy, flaky spots along the hairline. It can also appear on the eyebrows, eyelids, facial hair area, or T-zone.
Hairline psoriasis
This is scalp psoriasis that spreads to the face. It usually hits the forehead or ears the hardest. In severe cases, it can even lead to clogged ear canals.
We still don’t know the exact cause of psoriasis. But we do know it’s a chronic immune-mediated disorder, according to the American College of Rheumatology and National Psoriasis Foundation.
Psoriasis can happen when your immune system attack yours body’s cells. This can lead to a surplus of skin cells that build up on top of each other.
Research shows genetics also plays a role. You’re more likely to have psoriasis if it runs in your fam (like if one or both of your parents has it).
Here are some risk factors that can trigger a flare-up:
- stress
- smoking
- sunburn
- skin injuries
- heavy alcohol use
- cold or dry weather
- yeast infections (like Malassezia)
- certain meds (e.g. lithium, hydroxychloroquine, or prednisone)
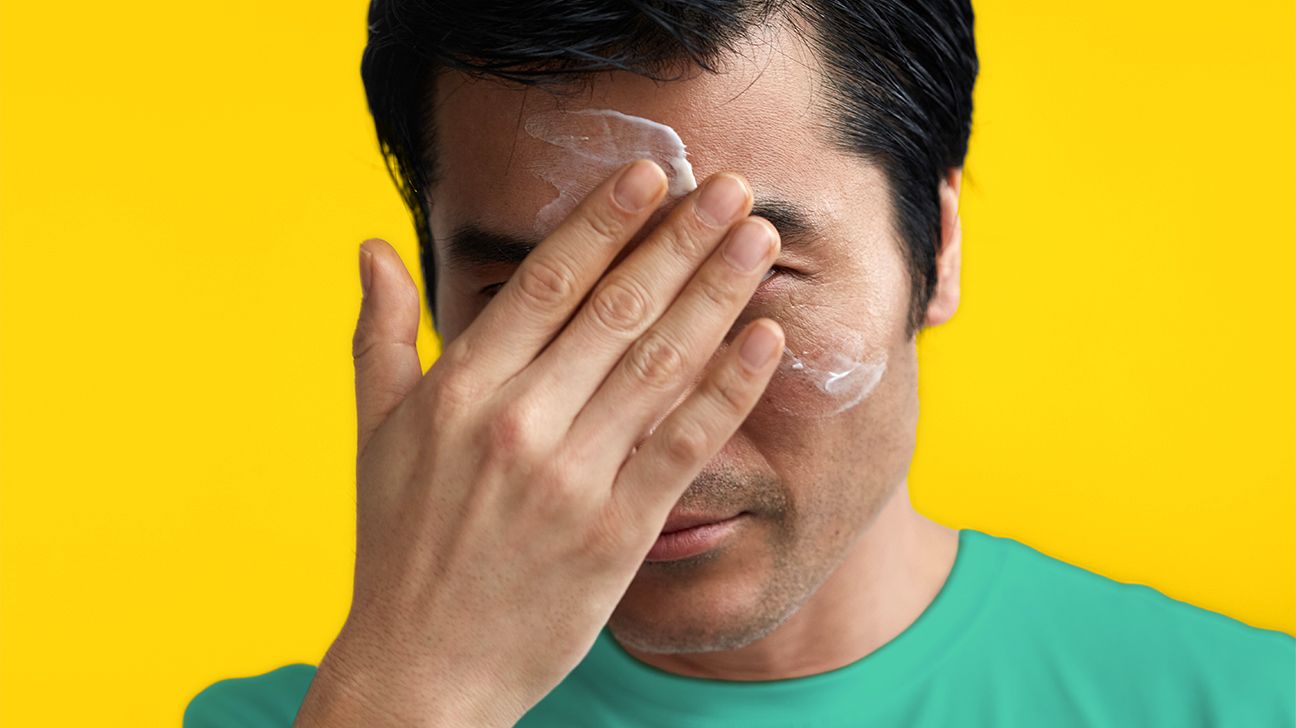
Facial psoriasis can be tricky to treat. The skin on your face is thinner and more sensitive than the rest of your skin. That means you have to be extra careful with your skin care.
Here are some of best treatment options.
Corticosteroids
Over-the-counter (OTC) topical corticosteroids like hydrocortisone can help reduce itching and discomfort. They can be applied directly to the skin, but you shouldn’t use them near your eyes.
PSA: Topical steroids can only be used as a short-term solution to ease symptoms. Overuse can lead to:
- thinning skin
- easy bruising
- easy-to-tear skin
- contact dermatitis
- changes in skin color
- inflamed hair follicles (folliculitis)
Other OTC options:
Your doc may suggest another type of OTC treatment if corticosteroids don’t work 10/10. This includes:
Scale lifters (keratolytics). They can help loosen and remove scales. OTC products that have lactic acid, salicylic acid, urea, or phenol can do the job. Just be sure to ask your doc before use as these can be quite irritating to skin on the face.
Anti-itch treatments. Products that have camphor, calamine, diphenhydramine hydrochloride (HCl), menthol, or benzocaine can help you ditch your itch. Just keep in mind some of these ingredients can cause dryness or irritation.
Occlusion. Some topical meds or creams can be occluded. This is when you apply a topical psoriasis treatment to the skin then wrap it with a medical dressing. Pro tip: This is a little hard to do on the face, but a clean cotton sock and plastic wrap can also do the trick 😉.
Biologics
Your doc might recommend a medication if your psoriasis doesn’t respond to other treatments. Biologics are a popular option. They help keep the immune system in check and can help prevent inflammation.
Your doc can administer biologics through injection or infusion. While it’s not a cure-all, it can slow psoriasis growth and slash your risk of flare-ups.
More meds
Biologics aren’t the only medication that can help curb your facial psoriasis. Your doc might prescribe:
- crisaborole (Eucrisa)
- tazarotene (Tazorac)
- tacrolimus (Protopic)
- pimecrolimus (Elidel)
- calcitriol (Vectical, Rocaltrol)
- calcipotriene (Sorilux, Dovonex)
DIY remedies and skin care
Skin care is self-care, fam. A bomb skin care routine can totes help you manage psoriasis symptoms.
Here are some DIY treatments that can help:
- Salicylic acid can slough off dead skin cells.
- Rinse with a saline solution to ease pain and discomfort.
- Look for soaps and shampoos designed with psoriasis in mind.
- Humectants (think glycerin and aloe vera) are hella good at hydrating your skin.
- Some oils (like hempseed oil or coconut) might help soothe sad skin. But there’s little research to back this up.
- Coal tar used to be one of the go-to remedies for psoriasis. But TBH, there’s little evidence to prove it’s legit.
- For sebopsoriasis in particular, it can be helpful to use anti-dandruff shampoos as face wash (just don’t get it in your eyes!).
P.S. Finding the right skin care routine will prob take some trial and error. So don’t worry if your skin doesn’t bounce back ASAP!
Lifestyle ch-ch-changes
Sometimes a simple tweak to your daily routine can make a big difference.
Here are some top tips:
- Adios stress! Stress is a major psoriasis trigger. Try to add relaxing activities — like meditation or yoga — to your routine to help you chill out.
- Keep away from triggers. Take note of any foods or activities that trigger a flare-up.
- No picking! We know the temptation is REAL. But picking and scratching at scales increases your risk of infection or bleeding.
- Hello hydration. Ask your doc which moisturizer can quench dry, scaling skin. They might suggest a medicated cream or an OTC lotion.
You’re not alone
Psoriasis can be emotionally taxing. It’s totally normal if the painful patches on your face make you feel self-conscious or even sad. But remember, you’re not alone ❤️.
There are TONS of online psoriasis support groups. You can also talk to a mental health professional or try a therapy app.
Reminder:
- You’re. 👏
- Amazing. 👏
- Just. 👏
- The. 👏
- Way. 👏
- You. 👏
- Are. 👏
- *hair flip*
If your skin is looking a little sus, it’s time to hit up your dermatologist.
It’s also a good idea to call your doc if you have:
- anxiousness about how your skin looks
- joint problems along with a facial lesions
- lesions that are heading toward your eyes
- discomfort that makes day-to-day stuff tough
- itchy, painful, or uncomfortable lesions on your face
Your dermatologist can see if it’s facial psoriasis. Then they can help you come up with a treatment plan.
