Any pain in your head can be a real pain in the ass. But why does your head hurt on just one side, behind your eyes, or near your neck in the first place?
Headaches are generally located in the front of the head and temples or on the side on the head. But the location of your headache can actually help tip you off to the cause of that persistent and annoying pain.
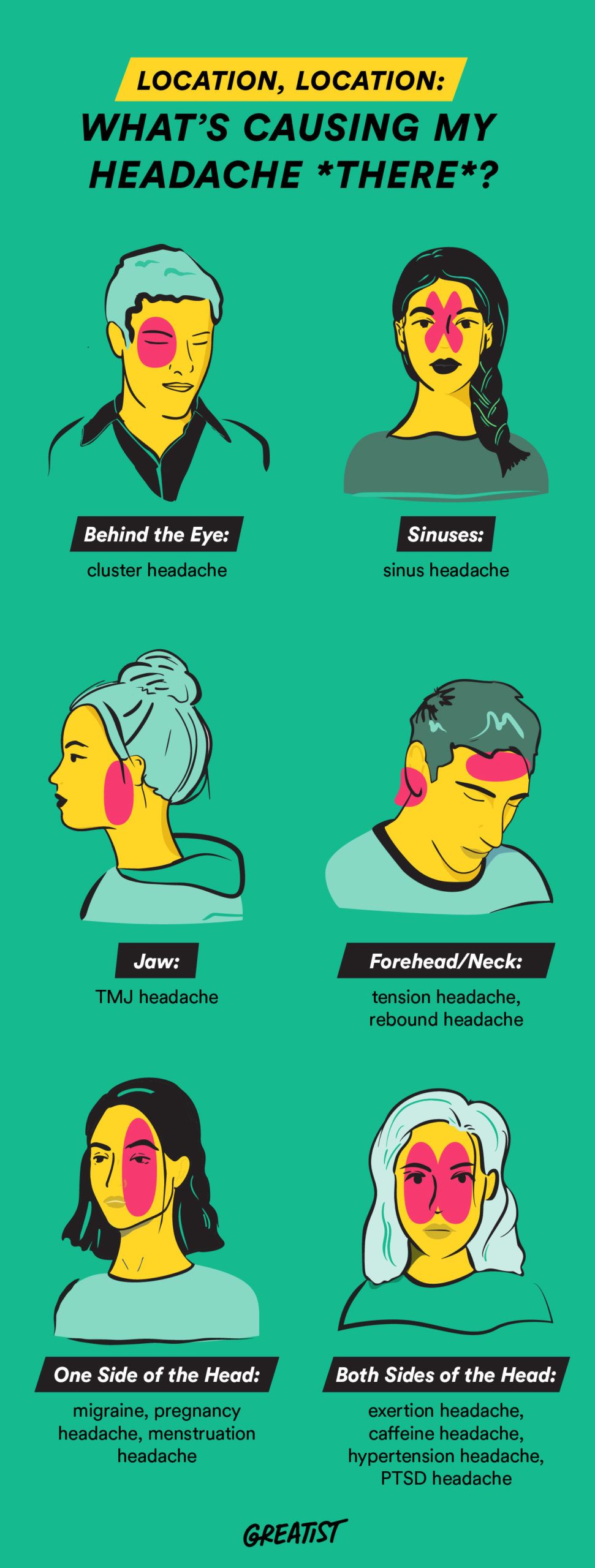
Here’s what the location of your headache may be trying to tell you and how to tell that headache byeee.
The World Health Organization reports that 1 out of every 20 people around the globe get headaches almost every day. Oof.
Headaches and their causes basically fit into one of two categories:
- Primary headaches. Caused by changes to nerves, blood vessels, and chemicals in the brain — totally unrelated to any underlying medical conditions.
- Secondary headaches. Caused by a condition, such as a head injury or an infection.
The secret to figuring out which type you have and how to treat it is tracking your symptoms. A good place to start your detective work is with your headache’s location.
| Top of head | Forehead | Back of head | One side of head | Both sides of head | Neck | Behind eye | Sinuses | Jaw | |
| Migraine | ✔️ | ✔️ | ✔️ | ✔️ | |||||
| Pregnancy headache | ✔️ | ✔️ | ✔️ | ||||||
| Menstruation headache | ✔️ | ✔️ | ✔️ | ✔️ | |||||
| Exertion headache | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ||||
| Caffeine headache | ✔️ | ✔️ | ✔️ | ✔️ | |||||
| Hypertension headache | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ||
| PTSD headache | ✔️ | ✔️ | ✔️ | ✔️ | |||||
| Cluster headache | ✔️ | ✔️ | ✔️ | ||||||
| Sinus headache | ✔️ | ✔️ | ✔️ | ✔️ | |||||
| Tension headache | ✔️ | ✔️ | ✔️ | ||||||
| Rebound headache | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | ✔️ | |||
| TMJ headache | ✔️ |
Here are some of the causes behind common headache hangouts.
One side of your head (or alternating sides)
Migraine attacks
Migraine pain often feels like a deep pressure within your head, with one side throbbing. You might also feel nauseated or be sensitive to light and sound.
This notorious headache monster is a savage that can last for days. Women are three times more likely than men to develop migraine. Those with depression or an anxiety disorder show an increased risk as well.
Pregnancy headaches
Got a bun in the oven? Pregnancy may be the culprit of that headache that starts on one side of your head. Your estrogen levels rise during pregnancy, and those hormonal changes can lead to headaches and migraine.
If you start to get headaches during pregnancy, make sure you get them checked out by a doctor before you assume they’re just “pregnancy headaches.”
If you’re prone to migraine attacks, pregnancy may also improve them or make them disappear.
Menstruation headaches
A visit from Aunt Flo can prompt a one-sided throbbing in your head. You might also feel nauseated and move into migraine territory, becoming sensitive to bright light and sounds.
Menstruation also affects your estrogen levels, which can give you a nasty hormone headache. The estrogen drop that happens just before your period may be to blame. Believe it or not, there are a few different types of these headaches (oh, joy).
Hormonal headaches also double down in women who already experience migraine. In fact, 60 percent of women who experience migraine symptoms also experience menstrual migraine (sorry, sis). Women with migraine typically report headaches before or during their period.
Both sides of your head
Exertion headaches
If you’ve been throwing weight around the gym (or around the bedroom) and you have a pounding headache on the sides of your head, you may be experiencing an exertion headache. This type of headache can be brought on by intense physical activities, causing that throbbing sensation.
Caffeine headaches
Drink too much or too little caffeine and you’ve got a caffeine headache on your hands. When you cut out caffeine, you’re withdrawing it from your routine, which can change your brain chemistry and trigger a headache.
On the flip side, caffeine in small amounts can be effective in treating headaches. It’s also part of headache medications like Excedrin.
Hypertension-associated headaches
Severe, uncontrolled high blood pressure, often called malignant hypertension, can contribute to headaches, although high blood pressure is not a common cause of headaches.
Hypertension headaches are very serious. If both sides of your head hurt and you have the following symptoms, that’s a warning bell to get to your doc ASAP:
- pulsating
- numbness or tingling
- vision changes
- nosebleeds
- worsening pain with activity
- chest pain
- shortness of breath
Some medications used to treat hypertension can cause headaches as a side effect, but not because of their effects on blood pressure.
In rare cases, hypertension can lead to bleeding of a blood vessel in the brain, which is a medical emergency. This may cause seizures and loss of consciousness soon after the headache starts.
On the other hand, low blood pressure (aka hypotension) from common problems such as dehydration or even blood loss due to menstruation can commonly cause headaches and lightheadedness.
Post-traumatic stress headaches
Those who have experienced post-traumatic stress have an increased risk of headaches.
These headaches sometimes happen after emotional trauma or a head injury — in fact, headaches are the most common complaint after a brain injury.
These headaches are thought to be related to the release of specific chemicals. Both sides of your head will hurt (it also feels like a tension-type or migraine headache). Sometimes just one side will hurt if the headache goes into migraine territory.
Post-traumatic stress headaches will be joined by other symptoms like:
- pulsating
- nausea/vomiting
- light/sound sensitivity
- worsening pain with normal activity
- dizziness
- insomnia
- poor concentration
- memory problems
- fatigue
- mood and personality changes like nervousness and depression
Behind your eye
Cluster headaches
You’ll typically feel cluster headaches behind or around your eye. They can also spread to your forehead, neck, nose, temples, teeth, or even shoulders on the same side.
While the cause of cluster headaches is unknown, men are twice as likely as women to experience them.
Cluster headaches can be even more intense than a migraine attack, and they can show up as often as eight times a day during a cluster period (which can be anywhere from 2 weeks to 3 months or more).
They’re also sneaky and can appear to have gone away for months or even years only to show up again later. And they love to arrive a couple of hours after you’ve gone to sleep.
The sinuses
Sinus headaches
Sinus headaches happen when your sinus passages (around your eyes, cheeks, forehead, and nose) become congested. Usually, this happens when you experience seasonal allergies or are sick.
You may also feel sinus headaches in other headache regions, but they’ll be most prominent in the sinus region, near your eyes.
It’s easy to confuse sinus headaches with migraine attacks. In fact, according to the Mayo Clinic, 90 percent of people who visit their doctor for a sinus headache learn that they’re actually experiencing migraine.
Migraine attacks and sinus headaches are treated differently, so checking in with your doc is a good move to find out which one you’re experiencing.
Sinus headaches can also be a symptom of sinusitis, an ongoing sinus condition. Before you start treatment, call your doc to narrow down what’s going on.
Forehead and/or neck
Tension headaches
Tension headaches usually feel like a band is squeezing your head, with the pressure toward your forehead. It’s common to also feel tension headaches behind your eyes and near your neck. Fatigue, stress, and anxiety are the most common triggers for tension headaches.
For most people, tension headaches are sporadic, happening maybe a couple of times a month, but for others they can be chronic.
According to the Cleveland Clinic, about 3 percent of the U.S. population has chronic tension headaches. Women are twice as likely as men to experience chronic tension headaches.
Rebound headaches
Your ex isn’t the only one on the rebound. These dull, tension-like headaches can sometimes be just as painful as migraine attacks. They usually occur on the front of the head, in the forehead area, but they can also occur along the neck and temples.
Rebound headaches are often brought on by overusing meds, typically over-the-counter (OTC) pain relievers. While you may be taking OTC pain relievers for headaches, using them too often may end up giving you more headaches.
If you aren’t taking OTC meds, rebound headaches can also be brought on by:
- stress
- hunger
- dehydration
- lack of sleep
- certain foods and drinks
Jaw/temples
TMJ headache
If you have pain near the top of your jaw and near your temples, it could be from temporomandibular joint (TMJ) pain.
The TMJ connects your lower jaw to your skull. If you have a jaw injury that affects the TMJ, or you were born with a structural issue there, you can get headaches from the muscles tightening.
Arthritis and grinding and clenching your teeth can also lead to TMJ pain.
Migraine treatment
At home
If you want to treat your migraine symptoms at home, you can try the following:
- Take OTC migraine meds.
- Rest in a quiet, dark space.
- Massage your scalp or temples.
- Apply cold compresses to the back of your neck or your forehead.
- Try herbal remedies like ginger.
Medical treatment
Your doctor may be able to help you manage migraine. Treatment plans depend on a few variables, such as your age, the type of migraine symptoms you experience, the frequency and severity of your symptoms, and any other medications you may be taking.
A doctor can prescribe migraine pain medication such as sumatriptan (Imitrex), rizatriptan (Maxalt), or rizatriptan (Axert).
A doctor can also prescribe migraine prevention medications like:
- propranolol (Inderal)
- metoprolol (Toprol)
- topiramate (Topamax)
- amitriptyline
Post-traumatic stress headache treatment
If you’ve had a brain injury or other post-traumatic stress that could be the root cause of your headaches, you’ll need to visit your doctor. A doctor and/or therapist can help you identify emotional triggers or suggest treatment plans to help with brain injury-related headaches.
Your doctor may suggest medication like:
- beta-blockers
- triptans, sumatriptan (Imitrex)
- amitriptyline
Tension headache treatment
At home
If you’re getting tension headaches, work on your posture and try to lessen eye strain (getting too much screen time?) to help relax the muscles around your neck and head.
Stay hydrated, eat a balanced diet, and get plenty of sleep. Also, cut down on alcohol and caffeine consumption and smoking (or even cut them out entirely) if you think they may be causing tension headaches.
Relaxation techniques like meditation or yoga may also help ease muscle tension. Of course, OTC pain relievers can also help you find relief in the moment, and at-home migraine treatments like cold compresses may help.
Medical treatment
Your doctor may suggest biofeedback relaxation techniques, cognitive behavioral therapy, stress management classes, or acupuncture.
You might also be prescribed a muscle relaxant, a selective serotonin reuptake inhibitor (SSRI), or another medication, such as indomethacin or naproxen.
Cluster headache treatment
At home
Cluster headaches may be brought on by factors such as lifestyle, weather, or diet. Cutting out alcohol, cigarettes, or food with nitrates (like bacon, hot dogs, and cold cuts) may help. You can also take an OTC pain reliever.
Medical treatment
Treatment by a medical professional is typically a two-step process:
1. Stop or control a current attack using a high dose oxygen mask (for up to 20 minutes) or a prescription nasal spray like sumatriptan to help ease the pain.
2. Prevent future attacks with daily medication like verapamil (which relaxes blood vessels), prednisone (which reduces inflammation), or anti-seizure meds.
Your doctor will know which medication is best for you.
Sinus headache treatment
At home
If your sinus headache is from allergies, avoiding known allergens and adding some aerobic exercise may help. You can also try some tried-and-true home methods for congestion, such as:
- using a humidifier
- spraying saline solution to clean the congested area
- inhaling steam
- applying a warm washcloth to the affected area for relief and drainage
- gently pressing on pressure points to loosen blockages from jammed mucus in your sinuses (Start with the bridge of your nose, between your eyes, and tap or apply constant pressure for about 1 minute.)
- OTC sinus headache medicine
Medical treatment
If at-home treatments aren’t enough, your doc may prescribe antihistamines, mucolytics (which clear out your mucus), or decongestants.
You likely won’t need antibiotics unless you have complications from sinusitis affected by a bacterial infection. But if your sinus headache is paired with severe sinus pain, call your doctor.
Pregnancy headache treatment
Talk to your doctor about medication and therapy options for pregnancy headaches, since many may be harmful to the fetus (even OTC pain meds aren’t safe).
You can also try safe home remedies for headaches like:
- resting in a dark, quiet room
- staying hydrated
- icing the pain
- doing breathing exercises
Period headache treatment
At home
Treatment techniques for menstrual headaches are similar to those for regular migraine symptoms:
- ice (Apply it to the painful spots, first wrapping the ice in a towel to avoid burn or irritation.)
- relaxation activities like yoga and acupuncture
- OTC anti-inflammatory drugs like ibuprofen
Medical treatment
A doctor can prescribe medications such as triptans, which block pain signals in your brain and can relieve headache pain in a couple of hours. Your doc may also suggest a combo of nonsteroidal anti-inflammatory drugs (NSAIDs) and triptan or other prescription pain meds.
Caffeine headache treatment
Caffeine headaches can last for a few days and can typically be treated at home. Try typical headache treatments like:
- taking OTC medication like ibuprofen, acetaminophen, or aspirin
- applying ice packs or cold compresses
- staying hydrated
Rebound headache treatment
Rebound headaches are progressive, which means they can get worse until the appropriate treatment is in place.
Over time, with repeated physical activity, these headaches could become longer. It’s best to see a doctor to rule out any underlying condition behind these headaches.
Typically, stopping the meds that may be causing the rebounds or at least lowering the dosage, along with preventive medication from your doctor, can help you manage these headaches. Sometimes, they may get worse before they get better.
Hypertension headache treatment
If you suspect you’re experiencing hypertension headaches, you need to visit your doctor for treatment.
These headaches typically disappear once blood pressure is better managed through lifestyle changes and medication. And they shouldn’t come back as long as your blood pressure is under control.
TMJ headache treatment
More research is needed to nail down a perfect treatment plan for TMJ headaches, but you can get short-term relief from NSAIDs. You can also try some helpful home remedies like:
- icing your jaw
- doing jaw exercises
- avoiding moving your jaw in certain ways (like clenching your jaw, yawning too wide, eating tough or chewy foods, or chewing gum)
- wearing a prescription mouth guard recommended by your dentist or doctor
If the suspected cause of your headache hasn’t already led you to see a doctor, there are other signs it’s time to seek medical help for your headache.
If your headache lasts more than 2 days and the pain only increases, or if you get headaches 15 or more days a month for 3 months, chat with your doctor.
If your headache comes with any of these severe symptoms, get to your doc ASAP:
- slurred speech
- stiff neck
- weakness in arm or leg
- rash
- confusion
- drowsiness
- vomiting
- facial numbness
- convulsions
- paralysis in any part of your body or vision loss
- fever of 100.4°F (38°C) or higher
Identifying the location and symptoms of your headache can be helpful in figuring out the cause.
OTC medications, home remedies, and lifestyle adjustments like staying hydrated may help you manage your headaches. If your headache points to an underlying health condition, visit your doctor for treatment rather than try at-home methods.
If your headaches keep coming back and you can’t find relief from home remedies, talk with your doctor about your options.

