It might seem a little freaky to think of sticking a birth control device up inside you and leaving it there for, like, years. But here’s the thing: When it comes to birth control, IUDs (intrauterine devices) are a real no-brainer.
“They’re safe, they’re effective, and they’re pretty much foolproof,” says Lauren Streicher, MD, associate clinical professor of gynecology at Northwestern University’s Feinberg School of Medicine.
The downside is that some IUDs have the potential to cause a few side effects worth mentioning.
To IUD, or not to IUD? That is the question many of us ask when pondering birth control. So we’ve put together a quick overview of the pros and cons of this pregnancy preventer.
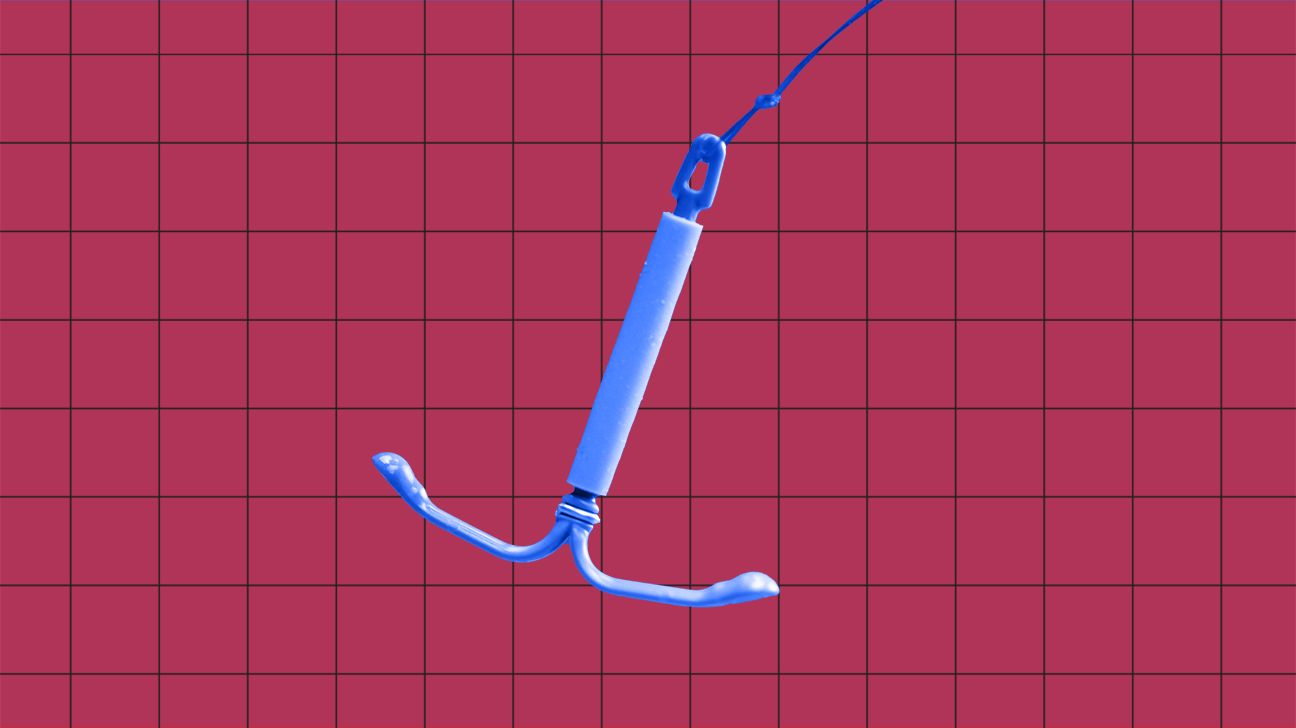
An IUD is a little T-shaped plastic or metal device about the size of a quarter. They’re no newbies, having been around since the 1960s. IUDs prevent pregnancy by releasing either copper ions or the hormone levonorgestrel, depending on the type.
Whether copper or hormone, they thicken cervical mucus, which blocks those little swimmers from sneaking in and implanting an egg. And that means no pregnancy worries (IUDs are about 99 percent effective) for at least 3 years (the copper ones can last for up to 10 to 12!).
Insertion isn’t too difficult. In about 10 minutes, your gynecologist can insert an IUD through the cervical opening into the uterus. Don’t worry, while it can feel a little weird, they have ways of making it less uncomfortable. Then you’re good to go!
If you’re over your IUD, there’s no problem with pulling it out early. You’ll be fertile again soon after its removed.
IUDs come in many types. Picking the model that’s right for you involves a talk with your gynecologist. If you’re considering an IUD, here are your choices:
1. Copper IUD: ParaGard
How it works: Sperm aren’t fans of copper, so they steer clear of the IUD. When they can’t reach the egg, there’s no fertilization in your future.
How long it lasts: It lasts up to 12 years.
Cost: $0 to $1,300 (depending on your insurance coverage), plus the cost of insertion
Added bonus: ParaGuard can be used as emergency contraception for those “oopsie” nights, and then left in place to protect against possible future mishaps.
Side effects: ParaGard is the only IUD that doesn’t make periods lighter. In fact, it may make them heavier — and more painful. In less than 1 percent of users, IUDs are linked to the infection pelvic inflammatory disease (PID).
2. Hormonal (levonorgestrel) IUD: Mirena, Kyleena, Skyla, and Liletta
How it works: Hormonal IUDs prevent pregnancy by making the cervical mucus thicker to prevent sperm from getting through and the uterine lining thinner to prevent implantation. Double duty protection!
How long it lasts: Up to 6 years (Mirena and Liletta), 5 years (Kyleena), or 3 years (Skyla). Your doctor will work with you to determine how long to keep the IUD in place based on shared decision-making.
Cost: $0 to $1,300 (depending on your insurance coverage), plus the cost of insertion
Added bonuses: Lighter, shorter periods are a major perk. Sometimes periods vanish altogether, making IUDs ideal for anyone with a heavy flow.
Side effects: Along with some unpredictable bleeding and spotting when it first goes in, breast tenderness, mood changes, weight gain, and acne are common.
1. They’re safe
This isn’t your mom’s IUD. Back in the ’70s, the popular Dalkon Shield gave IUDs a bad rep by increasing the risk of infections, complicated pregnancies, infertility, injuries, and death. Today’s IUDs are considered one of the safest birth control options.
2. They work
IUDs works so well that the American College of Obstetricians and Gynecologists (ACOG) — the organization your OB-GYN probably belongs to — touts them as the “most effective reversible contraceptive.”
With perfect use, the likelihood of pregnancy is 0.6 percent in the first year with a copper IUD and 0.2 percent with a hormonal one. That’s comparable to more permanent methods like sterilization.
In contrast, birth control pills and vaginal rings have failure rates of 7 percent, and for condoms it’s a whopping 13 percent.
3. They take the thought out of birth control
The IUD’s motto should be “Set it and forget it.” Other than doing quick checks to make sure the string is still there, you’re pretty much off the hook.
There are no pills to pop every day, and no condoms to unroll in the middle of a steamy romp. You can go years without giving your birth control much more than a passing thought.
4. They’re cheaper in the long run
Yes, an IUD will set you back up to $1,300 upfront (unless you have good health insurance, in which case it could be free). That might sound like a lot but, depending on your circumstances, birth control pills can cost up to $50 a month, which adds up.
Within a couple of years, the costs will even out. And from there, you’re off the financial hook for birth control.
5. You can likely say goodbye to heavy periods
For many women, the biggest upside to hormonal IUDs is that their periods get lighter. Eventually, Aunt Flo might bid you a fond farewell. So long tampons, hello white pants!
As with all things, this seemingly miraculous pregnancy preventer isn’t without its downsides. Here are a few.
1. Your bleeding could get wonky
While hormonal IUDs thin the uterine lining and bring a welcome lighter flow (or none at all), with the copper version, periods often get heavier and come with more painful cramps, especially in the first few months.
2. They won’t protect against STDs
If you haven’t settled in with a monogamous partner, you’re not going to get any protection from an IUD. To avoid STDs like herpes, gonorrhea, and HIV, stick with condoms until you’re in a one-on-one relationship and regularly testing.
3. Insertion isn’t fun
Since the IUD has to go up through your cervix, insertion isn’t going to be the most pleasurable experience of your life. You can have some period-like cramps or pain when it goes in. Taking ibuprofen or another pain reliever beforehand can make it more bearable.
4. It might be a pain afterward, too
After insertion, there may be some cramping for up to a couple hours. Bleeding is also common, so wearing a pad is a must.
If the cramps are I-can’t-move severe or bleeding is very heavy, go back to your doc to be sure the IUD is in the right place.
5. Perforation is a (very rare) problem
During insertion, there’s a very slim chance the IUD could slip and puncture — or perforate — the uterine wall, which requires surgery. Did we mention that the chance is really, really slim? The odds of this happening are only 1 in 1,000.
6. The IUD could slip out
About 2 to 10 percent of the time, the IUD falls out. This is more likely to happen if you’re under 20 or your periods tend to be heavy. If this does happen to you, it means you’re no longer protected against pregnancy.
Sometimes you’ll have more bleeding or pain, especially if the IUD is only partially out. Or there may be no warning that it slipped. That’s why it may be a good idea to stick a finger up there once a month and check that the IUD string is still hanging about a half inch out of the cervix.
The IUD still doesn’t match the birth control pill when it comes to contraceptive popularity, but it does have some notable perks. Once it’s in you can pretty much forget it, aside from a potential monthly string check if you doc recommends it.
IUDs are both super effective, and super safe. If you haven’t considered one of these T-shaped tools for pregnancy protection, it might be time to talk with your doctor and ask whether it might be right for you.

