Finding the right birth control can be as exhausting as swiping through Tinder. But if you’re thinking of swiping right on the Mirena IUD, it’s helpful to know the side effects before you make a commitment.
While this birth control method has big benefits — such as a bun-free oven — it also comes with possible side effects.
Mirena IUD side effects may include:
- weight gain
- acne
- sore boobs
- ovarian cysts
- moodiness
- cramps
- headaches
- irregular bleeding
- missed periods
Here’s everything you need to know about Mirena IUD side effects and how likely these effects actually are.
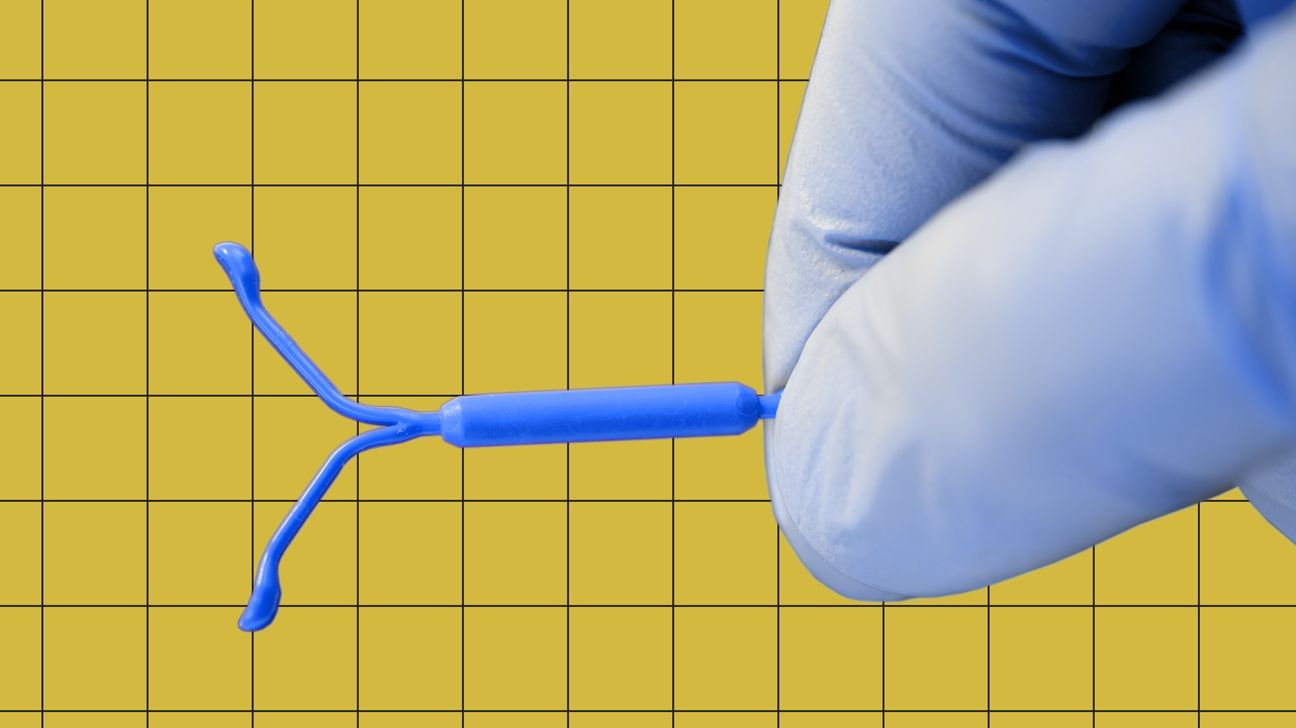
Mirena is a hormone-releasing intrauterine device (IUD) that’s placed in your uterus to prevent pregnancy or treat heavy periods (or to do both!). It looks like a tiny “T” and works by releasing small amounts of the progestin hormone levonorgestrel directly into your uterus.
Having a hormonal IUD is great for those who don’t want to worry about remembering to take a pill or get a shot. It can also help lessen or eliminate your period.
IUDs last for several years, and the Mirena can be left in for 5 to 6 years, depending on whether you’re using it mainly for heavy flow control or to prevent pregnancy.
Weight gain
There are a lot of reasons you might gain a few pounds, but Mirena likely isn’t one of them.
While some folks say Mirena causes weight gain, there’s not really any evidence to back this up. In fact, Mirena’s website doesn’t even list weight gain as one of the device’s common side effects.
Acne
IUDs are great at keeping your uterus clear, but keeping your skin clear? Maybe not so much. Hormonal IUDs, including Mirena, can likely lead to acne.
A 2008 review on the safety and side effects of Mirena noted that hormonal IUDs containing levonorgestrel (the main ingredient in Mirena) could increase the chances of experiencing acne.
Sore breasts
The boob pain you likely feel right around your period is the result of a swell in progesterone, a hormone your ovaries produce.
There’s no research on how commonly this soreness occurs while on Mirena. But, it would make sense if you were to experience this side effect, since the device releases progestin, a synthetic version of progesterone.
Ovarian cysts
Mirena may cause ovarian cysts to develop in some people. While these cysts will often go away on their own within 2 to 3 months, they can be painful.
Some cysts will require surgery, so talk with your healthcare provider if you start to have any pain or discomfort.
Mood changes
When looking at the link between hormonal birth control, like the Mirena IUD, and depression, the research is a bit mixed.
For a study on birth control and depression published in 2016, researchers collected data from 1 million participants over a 14-year period.
The study noted that people who used hormonal birth control methods were 1.4 times more likely to be prescribed antidepressants. But these results didn’t account for those who may have experienced depression but were not prescribed medication for it.
However, a study published in 2018 suggested that progestin-based birth control methods like Mirena do not lead to depression.
Think you need some help?
If you’re experiencing symptoms of depression, talk with your healthcare provider. They can help determine if the cause is your birth control or something else and help you explore your treatment options.
Cramping
Cramping is an annoying yet common side effect during insertion. Thankfully, the cramps should disappear within 30 minutes.
If you’re experiencing killer cramps more than 30 minutes after insertion or within the first few days afterward, contact your healthcare provider. Your Mirena may not be inserted properly, or something else may be at play.
Headache
According to Mirena’s website, headaches and migraine episodes (ugh) are common side effects. If you’re already prone to headaches or migraine, talk with your doc before choosing Mirena to determine if it’s the best option for you.
Irregular bleeding
Because getting a visit from Aunt Flo isn’t fun enough, you may also experience bleeding or spotting between periods during the first year you have a Mirena IUD.
This irregular bleeding may be heavier at first and then become lighter. But it should stop by the end of the first year. If you continue to have heavy bleeding, contact your healthcare provider to see what’s up.
Missed period
Period MIA? Before you worry, keep in mind that about 1 in 5 Mirena users stop getting a period within 1 year.
Still, it’s always best to be safe rather than sorry: If you think you may be pregnant, take a pregnancy test or contact your healthcare provider.
And don’t forget: Once you have Mirena removed, your regularly scheduled Shark Week will return as usual.
Ah, insertion. For some, this process is slightly uncomfortable. For others, it’s downright painful. The experience is like Forrest Gump’s box of chocolates: You never know what you’re gonna get.
According to the FDA, you may feel faint or dizzy or experience cramping while having Mirena inserted.
Once it’s in, you may have pain, dizziness, or bleeding. But Mirena’s website says these symptoms should disappear within 30 minutes.
When to call your doc
If the pain, bleeding, or dizziness doesn’t go away after 30 minutes, contact your doctor. The IUD may have been inserted incorrectly or may not be in the right place.
Call your doctor ASAP if you develop a fever or unexplained pain within a few days of insertion, as this could be a sign of sepsis. Sepsis is very rare but very serious.
The first year with a Mirena IUD may feel like a bit of a roller coaster as your body adjusts to this strange new tenant.
The first 3 to 6 months may bring irregular periods, longer or heavier periods, cramping, or spotting. As your body adapts to your IUD, you may still experience some of these effects, but they generally lessen over time.
By the time you celebrate your insertion anniversary, you may be having delightfully light periods. You may also be one of the 1 in 5 users the Mirena website touts as having no period at all by the end of the first year!
By year 3 (sometimes even year 2) and beyond, you should be experiencing fewer side effects. Your period should be lighter and less uncomfy, and you likely won’t be dealing with acne or sore boobs anymore (yay!).
On the flip side, you may still have occasional spotting or irregular periods (boo!).
Removing an IUD is fairly straightforward: Your healthcare provider will use a special instrument to secure the IUD strings and gently guide the IUD out of your uterus. You may have some cramps or bleeding during this process. Only rarely do more serious side effects or complications occur.
You may have irregular periods for the first few months after removal, but your flow should regulate in time.
If you’re looking to get pregnant, Mirena’s website says you can start trying right away once the device is removed. Not planning to put a bun in the oven? Make sure you start using other forms of contraception right away.
Mirena can be used for 5 to 6 years. After that, you’ll need to remove or replace it.
Prepare for a case of deja vu when getting a new Mirena inserted, as you’ll likely experience side effects similar to those you had the first time. Some folks say the second time comes with fewer side effects, but there’s no scientific proof of this.
Don’t forget!
If you had any major issues with your IUD, be sure to talk with your healthcare provider before getting a new one inserted, especially if your body expelled an IUD in the past (more on that in a moment).
PID
Pelvic inflammatory disease (PID) is a common infection that’s often (but not always!) caused by a sexually transmitted infection (STI).
According to the Centers for Disease Control and Prevention (CDC), you’re at a higher risk of developing PID in the first 3 weeks of having an IUD.
If you experience any of these PID symptoms, contact your healthcare provider ASAP:
- irregular bleeding
- pain during sex or during urination
- abdominal pain
- fatigue
- fever
- foul-smelling vaginal discharge
Expulsion
Much like expelling a student from school, your uterus may decide to expel your IUD (or shift it so it winds up in the wrong spot).
Be sure to check your IUD strings regularly to make sure it’s where it needs to be. Mirena recommends doing this monthly.
Contact your healthcare provider if you can’t feel the strings or if they feel longer than normal.
Perforation
In rare cases, an IUD can poke through the uterus — this is known as perforation. According to the American College of Obstetricians and Gynecologists, this happens in only 0.14 percent of hormonal IUD insertions.
You’re at a higher risk of perforation if your IUD is inserted when you’ve recently given birth or while you’re breastfeeding. The IUD will need to be surgically removed if it perforates your uterus and enters your abdominal cavity.
Pregnancy
Your chances of getting pregnant while on Mirena are fairly slim. But it is possible — 0.2 percent of Mirena users get pregnant within the first year.
Having an IUD while pregnant can affect your fertility and even cause a miscarriage. If you’re using Mirena (or any IUD) and think you’re pregnant, talk with your healthcare provider right away.
Hormonal birth control methods like the Mirena IUD have several benefits, but side effects are also possible. These effects can range from common experiences like spotting and acne to rare and serious (and rare) side effects like perforation.
Based on your unique situation, you may or may not experience side effects when using Mirena. If you have any questions or concerns or if you’re experiencing unpleasant symptoms, talk with your healthcare provider.

